Return to Contents | Previous >
Most publicly funded mental health and addiction services are funded through Vote Health. Approximately 9% of total Vote Health funding ($1.4 billion) was spent on mental health and addiction services in 2016/17.
The vast bulk of Vote Health funding set aside for mental health and addictions ($1.35 billion) is devolved to district health boards (DHBs) and is ‘ring-fenced’ within overall DHB funding.
The mental health ring fence was introduced following the Mason Inquiry (1995–1996) 233 to prevent mental health and addiction funding from being reallocated to other service areas in the DHB bulk funding environment. At the time, it was estimated that 3% of the population in a given year would have severe mental health and addiction needs. The level of mental health and addiction services to be provided was therefore benchmarked at 3%.
Specifc rules (last updated in mid-2018) set out what the mental health ring-fenced funding can be used for. They include:
• DHBs must maintain or increase mental health and addictions expenditure by applying at least demographic and cost-pressure adjustments each year
• funding must be used for specialist services for people with the most severe mental health and addiction needs
• DHBs must fund specialist services for at least 3% of the population; once that target is reached, DHBs may use any remaining funding for other mental health and addiction services. 234
It should be noted that these ‘specialist’ services are not provided exclusively by specialist clinicians. Instead, these services involve a range of providers and diferent workers, across a mix of non-governmental organisations (NGOs) and community groups and DHB provider arms. In 2016/17, $954 million was spent through DHB provider arms; $391 million through NGOs. The proportion of funding allocated to DHB provider arms and to NGOs has remained similar over the last 10 years (72% and 28%, respectively). 235
Details of the types of services that must be provided are set out in the service specifications for DHBs issued by the Ministry of Health. There are different specifications for different age groups, ethnicities and service types.
Specialist services can include acute and crisis services, community-based treatment and therapy services, and services to promote resilience, recovery and connectedness (for example, vocational support, living skills and housing coordination services).
Most specialist services are delivered in community settings rather than forensic or inpatient settings.236 In line with this, in 2016/17, forensic and inpatient services accounted for 22% of total ring-fenced expenditure. 237
The numbers of people accessing specialist services are set out in Figure 5 and Table 4.
Figure 5: Number of people accessing specialist services by age, 2008/09 to 2016/17 (data provided by the Ministry of Health)
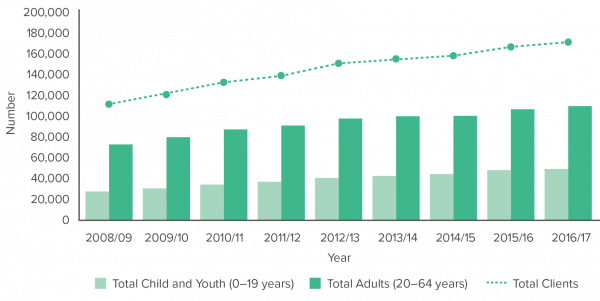
Table 4: Summary of specialist service access data, 2008/09 and 2016/17 (data provided by the Ministry of Health)
|
Category |
2008/09 |
2016/17 |
Change |
|
Total accessing mental health and addiction services |
111,734 |
171,693 |
54% |
|
Māori accessing mental health and addiction services |
23,762 |
46,322 |
95% |
|
Pacific peoples accessing mental health and addiction services |
6,038 |
9,942 |
65% |
|
Percentage of population accessing specialist care under ring-fence |
3% |
4% |
– |
Funding outside the ring-fence
Primary mental health
Outside of the ring fence, general primary care services are expected to meet mild to moderate and moderate to severe mental health and addiction needs.
‘General primary care’ encompasses a broad spectrum of services and providers, including both generalist services and primary mental health services. Key players include general practice (for example, general practitioners and practice nurses), school-based services, midwifery, Well Child Tamariki Ora, and NGO primary health services.
General primary care services are funded mainly through capitation from government (that is, a form of population-based funding) and co-payments from service users.
There is also approximately $30 million of additional funding (outside of the ring fence) specifically for primary mental health and addiction services (for example, counselling and extended GP visits). However, this funding is tightly targeted towards youth, Māori, Pacific peoples and people on low incomes.
We received data about the number of people accessing this funded care for one year (2015/16). In 2015/16, an estimated 106,000 adults (aged 20 and over) and 15,800 young people (aged 12–19) were seen by primary mental health services in New Zealand.
Nationally purchased activities
A further $100 million of nationally purchased services and activities is funded directly by the Ministry of Health through Vote Health. These services and activities include workforce development, adult inpatient and forensic services, and public promotion campaigns.
233 Committee of Inquiry into Mental Health Services (K Mason, Chair). 1996. Inquiry under Section 47 of the Health and Disability Services Act 1993 in Respect of Certain Mental Health Services: Report of the Ministerial Inquiry to the Minister of Health Hon Jenny Shipley. Wellington: Ministry of Health tiinyurl.com/y6w4nqr5.(external link)
234 Ministry of Health. 2016. Operational Policy Framework 2018/19 (version 28 August 2018). https://nsfl.health.govt.nz/accountability/ operational-policy-framework-0/operational-policy-framework-201819(external link)
235 Based on data provided by the Ministry of Health
236 Ministry of Health. 2017. Office of the Director of Mental Health Annual Report 2016. Wellington: Ministry of Health. www.health.govt.nz/publication/office-director-mental-health-annual-report-2016(external link).
237 Calculated based on data provided by the Ministry of Health.
< Return to Contents | Previous >
Last modified: